Health technologies in the global health context
Yu Cheng Hsu, PhD
Learning Objectives
- Understand digital health in the global health context
- Explore roles and applications of digital health
- Learn to design, implement, and evaluate digital health interventions
- Identify challenges of mHealth and telemedicine in global health
Digital Health
Digital Health: Definition
- Definition: The use of information and communications technology in support of health and health-related fields (WHO et al. 2017)
- An umbrella term that encompasses various information technology solutions for health
Discussion 1: Do global, start local
Local example of digital health
- Have you heard or tried any digital health product or service?
- how does it benefit your health ?
- Why do you use them ?
Fuel up digital health technology
- Technology
- Increasing coverage of internet and smartphone
- User engageement and empowerment
- People are more familiar with new technology
- Global health
- WHO recognized mHealth as a tool for enhancing healthcare systems Kay et al. (2011)
- Research, policy and business
- Economic potentials
Quadruple Aim of Digital Health
Proposed by Bodenheimer and Sinsky (2014):
- Improving the health of populations
- Reducing the cost of healthcare
- Improving the individual experience of care
- Improving the experience of providing care
Improving Population Health
Health Promotion and Education
- Health education initiatives
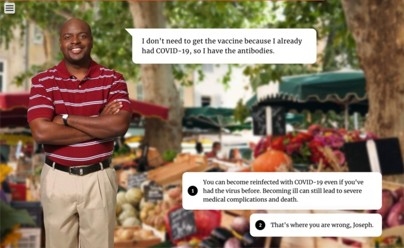
- Combating misinformation (Miller et al. 2024)
![Combating misinformation from Miller et al. (2024)]()
Disease surveillance
- Surveillance
- Targeting intervention (Gesicho and Babic 2022)
Personalized Devices and Behavior - Precision medicine - Promoting healthy behaviors
Reducing the Cost of Healthcare
Improving Individual Experience of Care
- Connected Care Integration:
- TB treatment adherence in India (Narasimhan et al. 2014)
- Just-in-Time Interventions:
- Alcohol overuse intervention for adolescents (Haug et al. 2020)
- Destigmatization:
- Digital platforms provide anonymity for sensitive conditions
- HIV (Mulawa et al. 2021)
- Mental health (Kim, Xu, and Wang 2022)
- Digital platforms provide anonymity for sensitive conditions
Improving Experience of Providing Care
- Telemedicine:
- During COVID-19 (Mahmoud, Jaramillo, and Barteit 2022)
- Mental health support Maha, Kolawole, and Abdul (2024)
- Integrated Healthcare Information:
- Healthcare information systems in Kenya (L. A. Celi et al. 2020)
Design, implement, and evaluation
Implement digital health product as a PM
Importance of Participatory Design
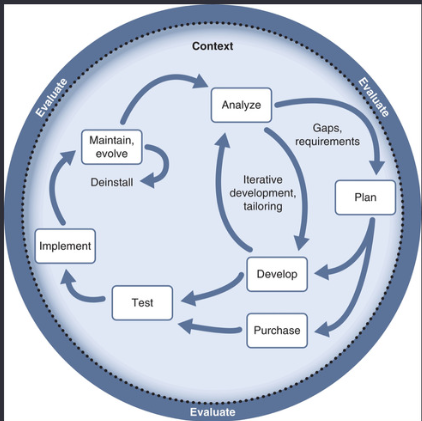
Nelson and Staggers (2013) proposed system life life cycle of health informatics
- Analyze
- Plan
- Develop
- Test
- Implement
- Maintain
- Evaluate
Participatory digital medicine design
Participatory design
Importance of Participatory Design
- Involves patients and professionals for better outcomes
- Aligns with P4 medicine goals
- predictive
- preventive
- personalized
- participatory
- Enhances communication and adherence
Through the participatory medicine approach
- Better health outcome
- Better communication
- Personalized design of intervention
- Higher adherence to the treatment
Non-Participatory Design Pitfalls
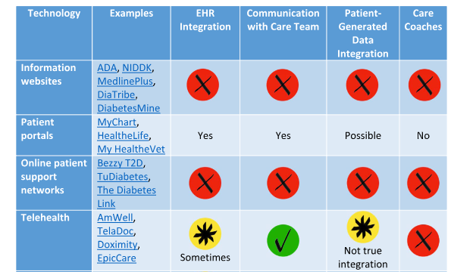
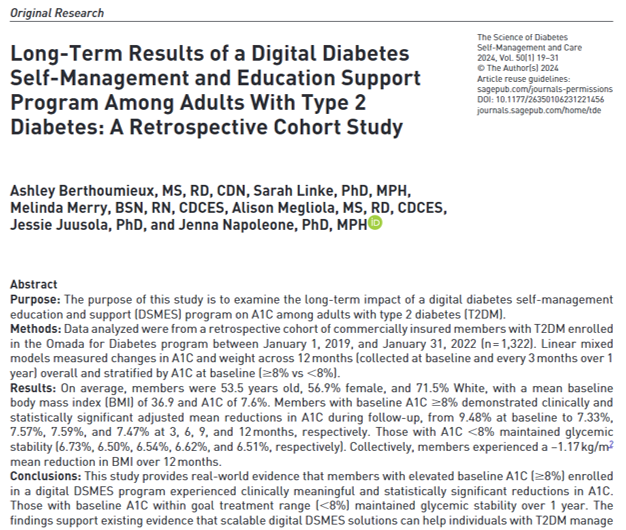
Participatory – example in diabetes
Intervention strategy
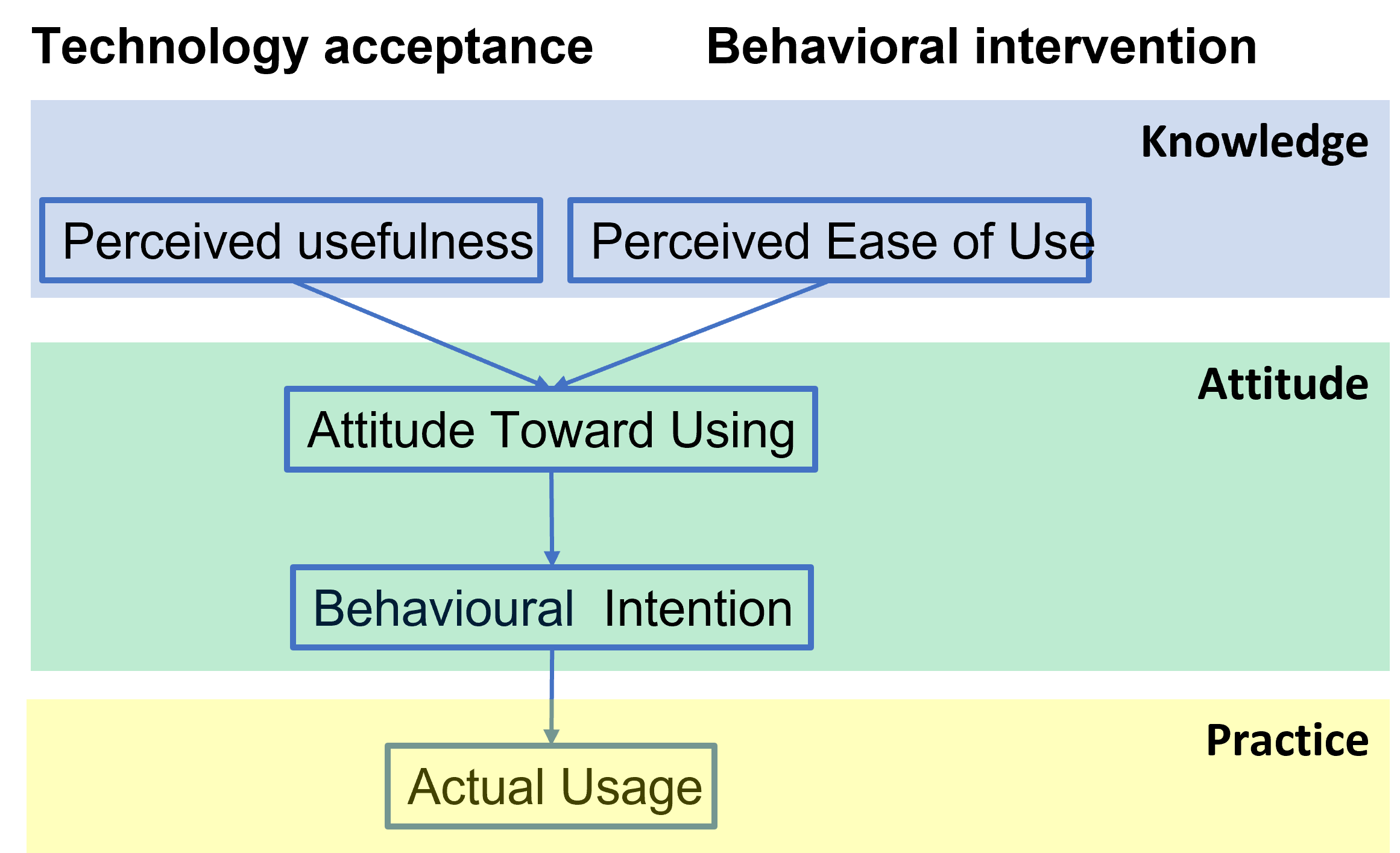
Intervention Strategy: Technology Acceptance Model (TAM)
Adopting new technology
- What new app/technology product/healthy lifestyle have you recently given up?
- What were your initial motivations for trying it?
- Why did you give up? How long did you sustain it before giving up?
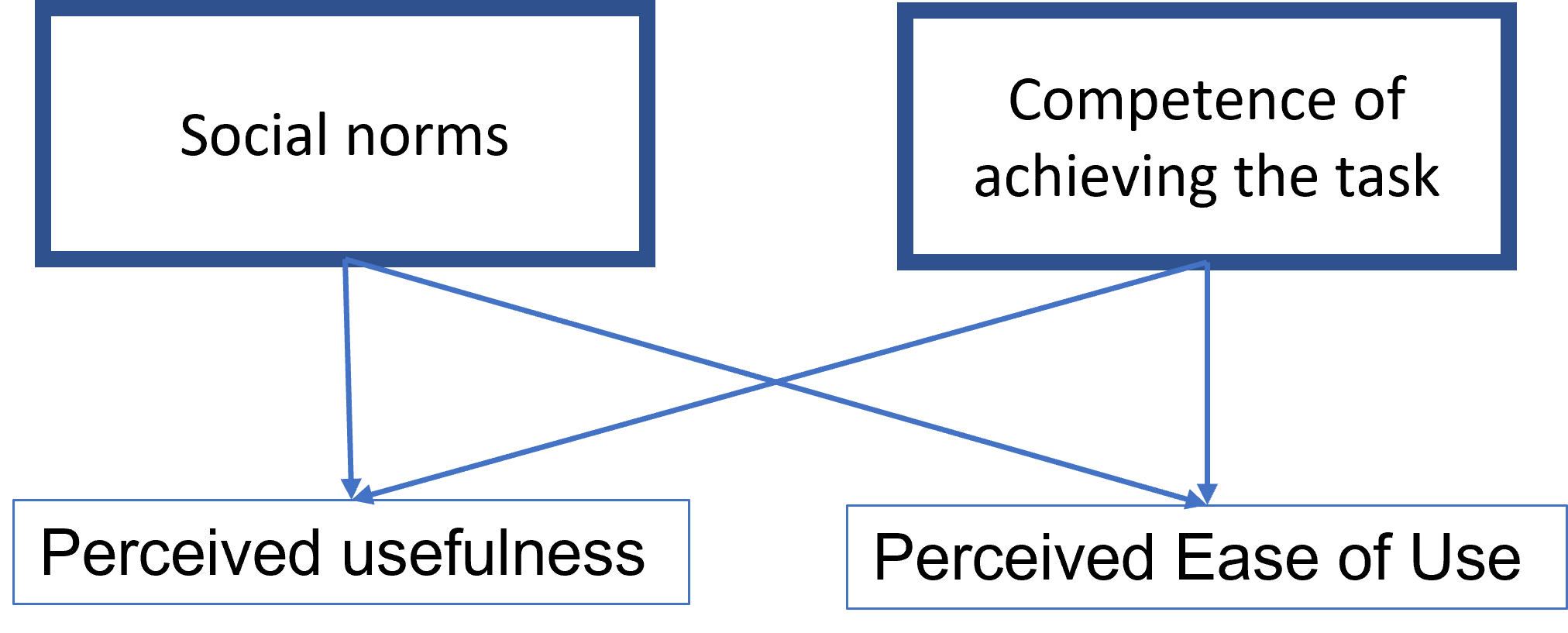
Intrinsic and extrinsic factors on TAM
From the TAM model, it is no clear how do we increase individual’s knowledge.
Venkatesh and Davis (2000) shows that social norms and competence are important in shaping user’s perception.
It suggest some direction of intervention
- Eliminating stigma and promotion
- Provide good quality of work
Evaluation
Evaluating Digital Health Interventions
- (Zhang et al. 2025) Three Dimensions of Evaluation
- Theme
- Stakeholders
- Stage
Stakeholder x Theme
Stage x Theme
Implementation Challenges in the Global Health context
- Policy
- Standardization
- Monitoring and evaluation
- Infrastructure
- Patients
- Urgency
- Attitude toward digital technology
- Service provider
- Training
- Attitude toward digital technology
Future of digital health
Further reading
The material covers in this slide is majorly referenced and L. A. G. Celi et al. (2017 - 2017)
Bibilography
Acharibasam, Jeremiah W, and Rolf Wynn. 2018. “Telemental Health in Low-and Middle-Income Countries: A Systematic Review.” International Journal of Telemedicine and Applications 2018 (1): 9602821.
Bodenheimer, Thomas, and Christine Sinsky. 2014. “From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider.” The Annals of Family Medicine 12 (6): 573–76.
Celi, Leo Anthony G., Hamish S. F. Fraser, Vipan Nikore, Juan Sebastián Osorio, and Kenneth Paik. 2017 - 2017. Global Health Informatics : Principles of Ehealth and Mhealth to Improve Quality of Care. Cambridge, Massachusetts: The MIT Press.
Celi, Leo Anthony, Maimuna S Majumder, Patricia Ordóñez, Juan Sebastian Osorio, Kenneth E Paik, and Melek Somai. 2020. Leveraging Data Science for Global Health. Springer Nature.
Davis, Fred D. 1989. “Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology.” MIS Quarterly, 319–40.
Davis, Fred D, and Viswanath Venkatesh. 1996. “A Critical Assessment of Potential Measurement Biases in the Technology Acceptance Model: Three Experiments.” International Journal of Human-Computer Studies 45 (1): 19–45.
Gesicho, Milka, and Ankica Babic. 2022. “Designing a Dashboard for HIV-Data Reporting Performance by Facilities: Case Study of Kenya.” In Advances in Informatics, Management and Technology in Healthcare, 238–41. IOS Press.
Haug, Severin, Raquel Paz Castro, Urte Scholz, Tobias Kowatsch, Michael Patrick Schaub, Theda Radtke, et al. 2020. “Assessment of the Efficacy of a Mobile Phone–Delivered Just-in-Time Planning Intervention to Reduce Alcohol Use in Adolescents: Randomized Controlled Crossover Trial.” JMIR mHealth and uHealth 8 (5): e16937.
Kay, Misha, Jonathan Santos, Marina Takane, et al. 2011. “mHealth: New Horizons for Health Through Mobile Technologies.” World Health Organization 64 (7): 66–71.
Kim, Hye Min, Yusi Xu, and Yunwen Wang. 2022. “Overcoming the Mental Health Stigma Through m-Health Apps: Results from the Healthy Minds Study.” Telemedicine and e-Health 28 (10): 1534–40.
Maha, Chukwudi Cosmos, Tolulope Olagoke Kolawole, and Samira Abdul. 2024. “Transforming Mental Health Care: Telemedicine as a Game-Changer for Low-Income Communities in the US and Africa.” GSC Advanced Research and Reviews 19 (2): 275–85.
Mahmoud, Kareem, Catalina Jaramillo, and Sandra Barteit. 2022. “Telemedicine in Low-and Middle-Income Countries During the COVID-19 Pandemic: A Scoping Review.” Frontiers in Public Health 10: 914423.
Miller, Emily, Alex Michel, Prachi Singh, and Rupali Limaye. 2024. “Countering Vaccine Misinformation: Designing a Learning Resource for Healthcare Workers in Eight Countries.” Vaccine 42: 126091.
Mulawa, Marta I, A Lina Rosengren, K Rivet Amico, Lisa B Hightow-Weidman, and Kathryn E Muessig. 2021. “mHealth to Reduce HIV-Related Stigma Among Youth in the United States: A Scoping Review.” Mhealth 7: 35.
Narasimhan, Padmanesan, Aishwarya Bakshi, Sathyapriya Kittusami, Suma Prashant, Dilip Mathai, Kasturi Bakshi, Chandini Raina MacIntyre, and Pradeep Ray. 2014. “A Customized m-Health System for Improving Tuberculosis Treatment Adherence and Follow-up in South India.” Health and Technology 4 (1): 1–10.
Nelson, Ramona, and Nancy Staggers. 2013. Health Informatics: An Interprofessional Approach. Elsevier Health Sciences.
Rivas, Homero, and Thomas Boillat. 2023. Digital Health: From Assumptions to Implementations. Springer.
Till, Sarina, Mirriam Mkhize, Jaydon Farao, Londiwe Deborah Shandu, Livhuwani Muthelo, Toshka Lauren Coleman, Masenyani Mbombi, et al. 2023. “Digital Health Technologies for Maternal and Child Health in Africa and Other Low-and Middle-Income Countries: Cross-Disciplinary Scoping Review with Stakeholder Consultation.” Journal of Medical Internet Research 25: e42161.
Venkatesh, Viswanath, and Fred D Davis. 2000. “A Theoretical Extension of the Technology Acceptance Model: Four Longitudinal Field Studies.” Management Science 46 (2): 186–204.
WHO et al. 2017. Global Diffusion of eHealth: Making Universal Health Coverage Achievable: Report of the Third Global Survey on eHealth. World Health Organization.
Zhang, Yunxi, Yueh-Yun Lin, Lincy S Lal, Jennifer C Reneker, Elizabeth G Hinton, Saurabh Chandra, and J Michael Swint. 2025. “Stakeholder-Driven Multi-Stage Adaptive Real-World Theme-Oriented (SMART) Telehealth Evaluation Framework: A Scoping Review.” The Lancet Regional Health–Americas 44.